Veins are blood vessels that help bring blood back to the heart. Increased pressure in the superficial veins can lead to the development of varicose veins.
Varicose veins can develop anywhere in your body, but the lower limbs are most commonly affected.
Many factors can increase your risk of developing varicose veins, including:
- heredity
- overweight
- old age
- pregnancy
- work requiring prolonged sitting or standing
Varicose veins can be treated with non-invasive methods, in a short time and without changing your usual rhythm of life. The main goal of treatment is to relieve symptoms, prevent complications and achieve good cosmetic results. Varicose veins are enlarged, can be deformed and cause pain. They are usually raised above the skin and convex, and also have a red or bluish color.
Varicose veins often occur because of an underlying condition known as chronic venous insufficiency. Varicose veins are very common, especially in women.
Predisposition to varicose veins
Varicose veins can occur in men or women of any age. Occurs more often:
- women who have had multiple pregnancies
- in postmenopausal women
- in men over 50
- in people of any age who have varicose veins in the family
- in men and women with jobs that require prolonged sitting or standing, such as nurses, teachers, drivers, etc.
What causes varicose veins?
Varicose veins usually develop in the legs because the veins in the legs have to pump blood to the heart against gravity.
Less common causes of varicose veins are phlebitis (inflammation of the veins) and birth defects of the veins. Varicose veins are usually caused by a condition called venous insufficiency.
- Venous valves. The veins in the legs have valves that prevent the backflow of blood. When the functioning of these valves is disturbed, the blood in the veins begins to accumulate and is not fully conveyed to the heart.
- Dilated veins. The veins enlarge and increased pressure leads to the development of varicose veins.
- Weakness of the walls of the veins. In addition, weakness in the walls of the veins (due to trauma or blood clots in the past) can also lead to valve damage and the formation of varicose veins.
What are the symptoms of varicose veins?
Many cases of varicose veins are asymptomatic, but visual signs of venous involvement include:
- Large, tortuous, bulging veins
- Swollen ankles, sore feet
- Feeling of heaviness in the legs, especially at night
- Telangiectasias (varicose veins) in the same area as the varicose veins
- Lipodermatosclerosis (hard fatty deposits under the skin)
- Change in skin color to bluish or brown on the shins and ankles
- Varicose eczema (congestive dermatitis) dry, itchy, red skin in the affected area
- leg cramps
- restless leg syndrome
How to treat varicose veins?
There are different types of treatment for varicose veins. The best treatment will depend on the structure of your venous system:
- Location and size of the affected vein
- Presence or absence of symptoms
- Presence of associated skin changes (eg, dermatitis, edema, ulceration, etc. )
Treating varicose veins without surgery is a top priority. Potentially effective treatments for varicose veins include:
- Sclerotherapy. The introduction of a special drug into the vein, which leads to the sticking of the walls of the vessel
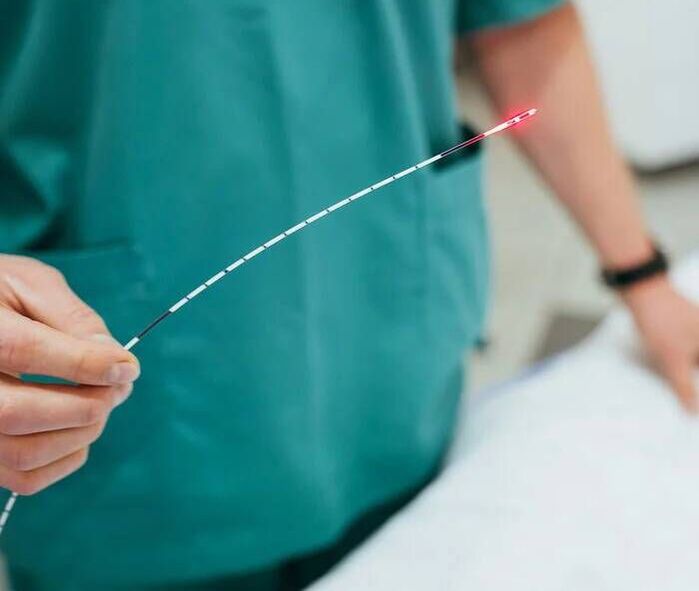
- Laser ablation Destruction of abnormal veins by radiofrequency, laser or other techniques
- Miniphlebectomy. Painless surgical treatment of varicose veins

Is it safe to treat varicose veins?
On the Internet, you can often see search queries such as "drugs for the treatment of varicose veins, ointment treatment for varicose veins, treatment of varicose veins at home or treatment of varicose veins with folk remedies". Such methods lack an effective evidence base, and self-treatment only delays high-quality treatment and worsens the condition of the veins.
Laser treatment of varicose veins is safe and convenient. The advent of minimally invasive therapy in the early 2000s led to a very favorable prognosis and minimal risks for most treatments.
It is important to contact a specialized phlebologist so that he selects an individual treatment plan that will be focused on the specific course of your disease.
How to diagnose varicose veins?
- Physical examination. A phlebologist performs a physical examination and takes a complete medical history, taking into account your symptoms and the state of your venous system.
- Ultrasound examination. To detect venous insufficiency, the doctor will prescribe an ultrasound. A venous ultrasound allows a complete evaluation of your venous system. The doctor will check if you have blood clots by seeing where the varicose veins are located.


What happens if varicose veins are left untreated?
If you do not experience any symptoms, you can control the condition of the veins without treatment. However, in some cases, varicose veins can lead to the development of blood clots or venous ulcers (sores that do not heal). Sometimes a varicose vein can rupture and cause heavy bleeding. If you have developed varicose veins, a consultation and examination by a phlebologist is recommended.


















