Venous pathologies in women are a common phenomenon. Gender is determined by hormonal changes, lifestyle characteristics, body functionality and other factors. Veins can be damaged under the influence of external and internal factors. This leads to stretching of blood vessels, thinning of the walls, plaque formation, valve dysfunction, blood thickening and other negative consequences. Varicose veins of the small pelvis in women are a type of venous pathology. It is characterized by discomfort, pain, a feeling of heaviness and pinching, and sometimes even leads to dysfunction of the reproductive system.
What are varicose veins of the small pelvis
Phlebeurismis a pathology characterized by a change in the normal state of the vessels and veins of the human body. ICD-10 does not have a separate classification. Venous diseases are designated by the code I80-I89. A separate classification includes varicose veins of the lower extremities (I83. 9), which are often associated with varicose veins of the small pelvis in women.
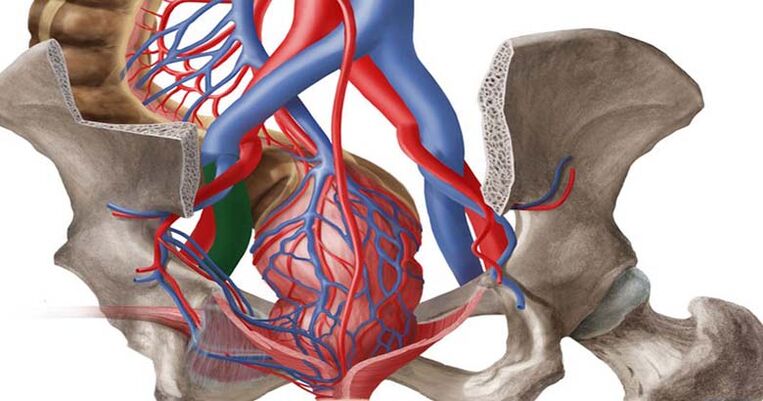
With varicose veins of the small pelvis, thinning of the walls of blood vessels, their expansion and stretching occurs. In this state, blood stagnates. Due to the decrease in tone, the vessels are not able to fully function and pump blood, which leads to the formation of peculiar nodes, commonly called varicose veins.
In recent years, a trend towards rejuvenation of the disease has been observed. If previously, varicose veins of the small pelvis mainly affected elderly women, now the pathology is found more and more in young patients. According to statistics, up to 20% of women of childbearing age have varicose veins of varying degrees. Pelvic varicose veins (PVVD) are often accompanied by other pathological processes, which seriously complicates the diagnostic procedure.
Varicose veins affect the functioning of the pelvic organs. May be accompanied by severe symptoms or show no clinical manifestations. In difficult situations, this becomes a cause of complications. Treatment of varicose veins is chosen individually and does not always achieve the desired result.
Classification of varicose veins of the small pelvis
Pelvic varicose veins occur differently in different women. Some patients complain of severe symptoms, while others have practically no pathological manifestations. For some, even serious treatment does not allow them to completely get rid of the pathology, while others can easily cope with the disease through lifestyle changes. In gynecology, a classification of varicose veins of the small pelvis has been adopted, which accurately characterizes the course of the pathology.
Forms of varicose veins of the small pelvis
Varicose veins of the pelvis in women are accompanied by a decrease in the tone of the vascular wall, weakening, decrease in elasticity and the formation of ectasia - an increase in lumen in one arealimited vein.
There are two forms of pelvic varicose veins:
- Varicose veins of the vagina and external genitalia (perineum)- characterized by a change in the structure of the channels of the great vein, as a result of which the external genital vein is affected. The cause is often long-term pregnancy, during which compression of the inferior vena cava and iliac vein occurs through enlargement of the uterus.
- Venous congestion syndrome- characterized by the expansion and stretching of the veins inside the small pelvis and the return of blood through them. The causes of such reflux can be very diverse.
Stages of varicose veins of the small pelvis
Varicose veins of the pelvic organs can occur in three stages. As the disease progresses, one stage replaces another. The stages of the disease differ in the severity of symptoms and the severity of the disease.
- First stage
Characterized by dilation of veins up to a diameter of 5 mm. Vascular tone decreases and the mesh takes on a tortuous appearance.
- Second step
It is characterized by a reduction in the elasticity of the vascular bed of the pelvis. The diameter of the dilated veins is 6 to 10 mm. The parametrial vessels and ovarian plexuses are affected.
- Third step
Characterized by total damage to the vascular fiber. The expansion diameter exceeds 10mm. Against the background of progressive varicose veins, a woman may develop complications.
Nature of development
Depending on the nature of their appearance and their evolution, varicose veins of the small pelvis are classified:
- Primary varicose veins of the pelvic veins in women
It forms in the context of acquired or congenital valvular pathologies. Doctors generally speak of valvular insufficiency of the veins, which is accompanied by the appearance of tortuous and overstretched vessels. Often the causes of primary varicose veins are increased physical activity, complications during pregnancy and childbirth, and the use of hormonal drugs.
- Secondary varicose veins of the pelvic veins in women
Formed against the background of past illnesses. Infectious pathologies, tumor processes, pelvic endometriosis and abnormal development of the pelvic organs can affect the tone of the veins.
Causes of the development of varicose veins of the small pelvis
Pathologies of the veins of the pelvic organs can develop for the following reasons:
- Heredity. Often, venous diseases in women are hereditary. If a mother, grandmother or aunt in the family suffered from varicose veins, the disease would likely affect the next female generation.
- Connective tissue dysplasia of the pelvic organs. This is a congenital anomaly characterized by a decrease in collagen production, against the background of which the tone of the vascular pattern decreases.
- Pregnancy. During pregnancy, the load on muscles and blood vessels increases significantly. The growing uterus puts pressure on nearby tissues and adjacent veins. In case of polyhydramnios, multiple pregnancies, large fetuses and other conditions, a woman may develop varicose veins.
- Excess body weight. With obesity in women, the pressure on the pelvic organs increases. This can lead not only to the development of varicose veins, but also to other health problems.
- Decrease in physical activity. The human body needs regular physical activity. We're not talking about grueling workouts. On the contrary, excessive physical activity can become an independent cause of varicose veins of the small pelvis. With a sedentary lifestyle, blood flow in the pelvis is disrupted and stagnation processes develop.
- Hormonal disorders. The work of the entire female body is entirely subject to hormonal levels. Hormonal changes and taking hormonal medications can lead to a decrease in vascular tone.
Varicose veins of the lower limbs are often accompanied by varicose veins of the small pelvis. If a woman has tortuous vessels in the legs, she should definitely undergo an examination of the pelvic vessels and, if necessary, undergo treatment.
Risk factors
The risk of developing varicose veins of the small pelvis in women increases with the following factors:
- bad habits;
- binge eating;
- disruption of the gastrointestinal tract and tendency to constipation;
- lack of intimate life;
- difficult pregnancy;
- surgical interventions;
- injuries to the pelvic organs;
- hormonal treatment;
- intense physical activity.
Symptoms of varicose veins of the pelvic organs
Many women have no symptoms of pelvic varicose veins. The disease can exist for a long time without clinical manifestations. At the same time, the pathology is insidious in that it progresses imperceptibly, leading to serious health problems.
The signs of varicose veins of the small pelvis in women may be similar to those of other gynecological pathologies. Therefore, when choosing treatment tactics, it is necessary to carry out differential diagnosis and exclude other diseases of the pelvic organs.
General symptoms of varicose veins of the small pelvis:
- pain in the lower abdomen;
- breakthrough abnormal uterine bleeding;
- discharge that has nothing to do with the menstrual cycle;
- a feeling of distension and the presence of a foreign body in the pelvis;
- lumbago in the sacrum, lower back, leg, perineum;
- bright premenstrual syndrome;
- severe pain during menstrual bleeding;
- discomfort and pain during intimacy;
- frequent urination;
- dysfunction of the digestive tract.
A characteristic sign of pelvic varicose veins in women is the formation of tortuous bluish veins in the external genitalia and in the vagina.
Diagnosis of pelvic varicose veins
A preliminary diagnosis can be made based on the patient's complaints and clinical examination. Visually, varicose veins look like cyanotic lymph nodes and dilated vessels. Since signs of pathology are often confused with other gynecological diseases, to clarify the diagnosis, it is necessary to carry out diagnostics:
- visual examination of the external genitalia;
- speculum examination of the vagina and cervix;
- palpation and diagnosis of valve functionality in the groin area;
- Ultrasound of the pelvic organs;
- Doppler study;
- CT scan;
- magnetic tomography;
- hysteroscopy;
- laparoscopy.
Treatment of varicose veins of the small pelvis
Treatment of pelvic varicose veins in women can be surgical, conservative or complex. The method of treatment is chosen individually, depending on clinical manifestations, stage of varicose veins, cause of development of venous pathology and other factors. The main goal of treatment is to reduce the symptoms of the disease and improve quality of life.
Drug treatment of varicose veins of the small pelvis
For varicose veins of the small pelvis, the doctor selects an individual treatment regimen. The following medications are traditionally prescribed:
- Venotonics. Modern pharmacology offers many types of venotonics. The main task of drugs is to increase the elasticity of blood vessels, normalize blood flow and stabilize the functioning of the valves. Medicines can be used both for internal use and in the form of ointments.
- Anti coagulants. The medications are prescribed for blood thickening due to pelvic varicose veins. This parameter is determined by laboratory tests. Anticoagulants prevent blood clots from forming and reduce the thickness of the blood.
- Non-steroidal anti-inflammatories. The drugs are used for severe pain and as an additional remedy for the inflammatory process. As a rule, NSAIDs have a symptomatic effect. They relieve the signs of varicose veins of the small pelvis, but do not completely solve the problem.
- Vitamin and microelement complexes. Since most people suffer from nutrient deficiencies and do not consume enough, supplemental vitamin intake is recommended. For varicose veins, it is recommended to take vitamins B, C, D.
Surgery
If drug treatment fails, it is recommended to consider the possibility of surgical treatment of pelvic varicose veins. The operation is also performed for severe forms of varicose veins.
A modern method of treating dilated veins is endovascular embolization of gonadal vessels. The procedure is performed in a hospital setting under general anesthesia. The operation consists of inserting spirals that block the conduit using a catheter into the dilated vein. As a result, blood flow completely stops in the pathological area. It should be noted that the operation is safe from the point of view of damage to the circulatory system. As the dilated veins themselves are pathological and can no longer function properly, it is advisable to exclude them from the general circulation. Refusal of treatment is accompanied by an increased risk of blood clots forming in the vessels.
The endovascular embolization procedure solves the problem of varicose veins of the small pelvis in 95% of cases. In the future, the woman is recommended to undergo lifelong prevention of vascular diseases.
General recommendations for women suffering from pelvic varicose veins
At any stage of treatment of varicose veins, as well as after completion of the correction technique, doctors recommend women to wear compression clothing. After the operation, the duration of use of this jersey is determined individually. Usually, in the first days after surgery, stockings are worn around the clock. In the future, it will be allowed to remove compression during sleep.
It is not recommended for women with pelvic varicose veins to play strenuous sports or carry weights. Baths, saunas and hot baths should be completely avoided. Thermal procedures can aggravate the course of varicose veins.
In case of varicose veins, special attention should be paid to body weight. Excess weight can become a stimulator of varicose veins. It is therefore important to stabilize your weight and lead an active lifestyle.
Why are pelvic varicose veins dangerous for women?
Complications of varicose veins:
- thromboembolism;
- thrombophlebitis;
- vein thrombosis;
- hemorrhoids;
- hormonal imbalances;
- abnormal uterine bleeding;
- chronic pelvic pain;
- infertility.
Pregnancy and varicose veins of the small pelvis
Varicose veins are generally not a cause of infertility. Enlarged and distended veins can be an increased risk factor for women planning to conceive. It is impossible to say right away how the body of the future mother will behave. The uterus is the main organ of the unborn child. If the blood flow in the reproductive organ is impaired or the blood circulation of the placenta is obstructed, then there is a high risk of miscarriage or the formation of various intrauterine disorders.
Prevention of varicose veins of the small pelvis
There is no specific prevention of varicose veins of the small pelvis. Every woman is at risk of developing varicose veins. Therefore, everyone must follow simple rules:
- healthy lifestyle;
- Good nutrition;
- obesity prevention;
- rejection of bad habits;
- moderate physical activity;
- drink enough fluids;
- refusal to wear high heels for a long time;
- a rational approach to pregnancy planning and prevention of pregnancy complications;
- the use of compression garments with a high risk of varicose veins;
- regular and scheduled medical examinations.
If varicose veins of the small pelvis have already been detected, the doctor will give recommendations on how to prevent the progression of the disease. As a rule, a woman is prescribed a course of venotonics and regular wearing of compression clothing.


















